Featured | Oct 9, 2024
Addressing Physician Burnout: Essential Steps for CME Tracking
Physician burnout, affecting 38% of US doctors, needs addressing to safeguard patient care. Reducing workload and adopting innovative solutions are crucial steps.

Featured | Oct 9, 2024
Physician burnout, affecting 38% of US doctors, needs addressing to safeguard patient care. Reducing workload and adopting innovative solutions are crucial steps.

Physician burnout is a real problem in the medical community. The term “burnout” was first used in psychology in 1974 by Herbert Freudenberger, and referred to the increased cynicism, emotional exhaustion and depersonalization that was experienced by workers. In a recent 2012 JAMA study, 37.9% of US physicians had high emotional exhaustion, 29.4% had high depersonalization and 12.4% had a low sense of personal accomplishment. Why is it important to address this burnout problem? Would you want a burnt-out veterinarian operating on your dear family dog? How about a burnt-out surgeon performing his 12th bypass of the week? We need reforms to the current healthcare system – from policy to education – that will allow physicians to perform to the best of their abilities, while decreasing the likelihood of burnout.
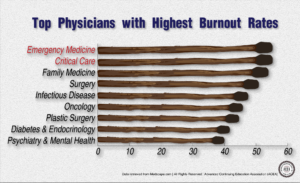
Emergency medicine remains the specialty with the highest burnout rates and if you’ve managed to watch one single episode from the 20 seasons of ER, this makes sense (only half-joking). In a study published by Medscape, emergency medicine physicians maintained the title of most burnt out specialty. On the other end of the spectrum, professions such as psychiatry and dermatology have significantly lower burnout rates. Part of this cynicism is instilled early on – I had a professor in college, Arthur Kleinman, who would always call the first year of medical school, before the clinical rounds, the pre-“cynical” years. It was a joke he made twice a semester, but really illustrates the problems with medical education and the profession as a whole.
One problem is that we see doctors as these steely super-humans, but they are people just like anyone else. Part of why burnout happens is our own depersonalization of physicians, as they are now often seen as cogs of a medical system that has been pimping them to maximize profits. With doctors currently being paid on a fee-for-service basis, there is an incentive for hospitals to have doctors become these uber efficient doctomatons (I should trademark that). During the pre-“cynical” years, young medical students probably wouldn’t imagine that their days would consist of seeing five people an hour for 10 hours a day.
The Atlantic feels like it has the answer to this problem, by proposing that the cure to burnout is remembering why physicians chose their career path and holding hands while singing Kumbaya with their medical staff (I might be paraphrasing). While an emphasis on the positive aspects of the profession is important, it does nothign to address the rot – that physicians are often over-worked and under-appreciated in our society. All the healthcare policy in the world is useless without the expertise and sacrifice of doctors – and if you’re upset by their salaries, look at the money insurance companies are raking in.
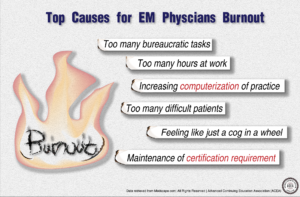
In addition to decreasing work load (which can be accomplished by increasing the supply of new physicians), we can also reduce their day-to-day stress through innovative medical applications. Now, in a normal blog post, I’d break off into a “top 7 best m-health apps 2016” section, but this is a serious issue…although if interested, I’ve included some at the bottom of this post. Another way we can reduce burnout is by hiring more data clerics. The modern doctor today is both a physician and data cleric, and while software from companies such as EPIC and Cerner claim to make things more efficient, they can in fact drive some practitioners into an early retirement, such as an unnamed doctor in a Boston Globe piece, who retired from her job at Boston Brigham and Women’s Hospital after Epic’s EHR was implemented.
Despite the undisputed status as the world’s superpower, the US can do better on many healthcare fronts, including cost, access and quality. Our quality rankings consistently rank below many other developed nations, which as a country who strives to be the best, is unacceptable for its people and for its reputation. One way we can improve quality is by decreasing the burnout rate of physicians. When you have some specialties with burnout rates greater than 50%, then you’re essentially rolling the dice with your healthcare, which is something that we should not have to do. We need to both stress the positive aspects of the practice, as the Atlantic suggests, as well as reducing the stressors that are burdening many physicians and fizzling out their flame for medicine.
Read More: Pediatric Nurses Need to Be Equipped to Treat LGBT Patients, Should Physicians Disclose Genetic Biomarker Results, Alaska CME Requirements 2017